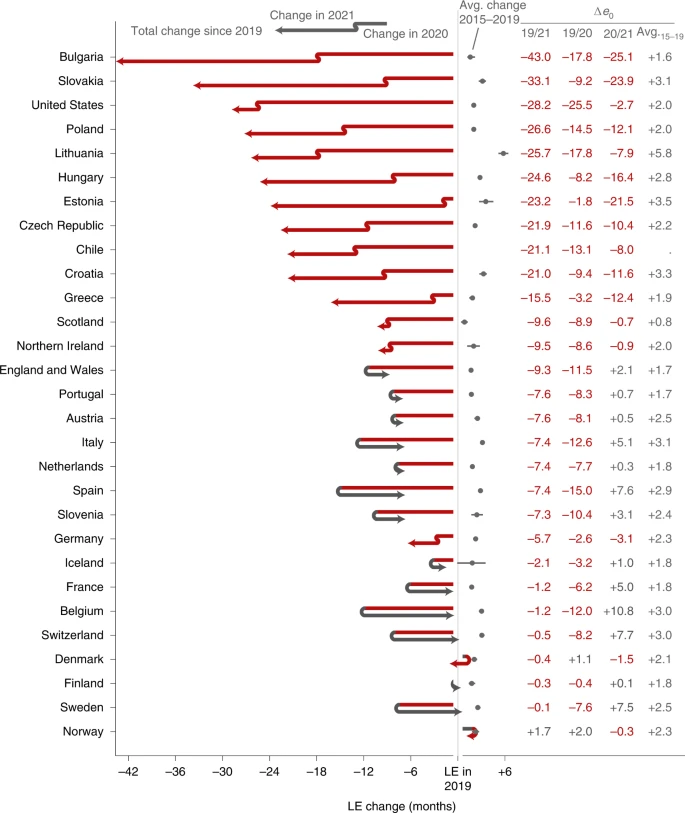
Covid-19 and Life Expectancy Rates
A study of 29 countries shows the impact of the pandemic.
Via Nature: Life expectancy changes since COVID-19. The study looks at 29 high-income countries (most of Europe, the US, and Chile). This is just additional evidence of the impact of the pandemic. The US’s comparative showing is noteworthy, as it is a further indictment of the policy approaches seen at the time.
The COVID-19 pandemic led to global increases in mortality and declines in period LE [life expectancy] that are without precedent over the past 70 years. The scale of these losses was clear by the end of 2020. By the end of 2021, it was clear that the pandemic had induced a protracted mortality shock in the United States and many European countries, measured as either compounded LE losses or persistent LE below pre-pandemic levels. Even the best-performing countries were lagging behind their LE projections for 2021 given a continuation of pre-pandemic trends.
So, yet again, clearly not just a little flu or the sniffles.
If the numbers look like this for wealthy countries, one suspects they are much worse for middle-income and poor countries. It will likely take years of research to fully see the impact.
The piece notes that US deaths were likely also linked to existing trends, neither of which is encouraging (i.e., overdoses and deaths from gun violence):
In the United States, the pandemic has accentuated the pre-existing mid-life mortality crisis. This is clear from the strong contribution of increasing mortality below age 60 to LE losses in 2020 and 2021. Because non-COVID mortality also increased in these ages, this may be interpreted as the continuation and worsening of a pre-existing mortality crisis among working-age adults31. In 2020, the largest share of non-COVID excess deaths in US males was from external causes (primarily due to drug overdoses and homicides), nearly 80% of which occurred at working ages32. Preliminary data show continued increases in deaths due to drug overdoses in 202133. However, part of the effect may be due to the under-registration of COVID-19 deaths among the working-age population. Differences in vaccine uptake by age may also have contributed to the shift to younger mortality in the United States. By 1 July, when vaccines were already available in the United States, only 66.9% of 50- to 64-year-olds were fully vaccinated compared with 82.3% of 65- to 74-year-olds (as per the COVID Data Tracker of the Centers for Disease Control and Prevention). This means that older age groups were better protected during the large Delta wave in the United States in the summer/autumn of 2021 than during previous waves. Pre-pandemic differences in underlying conditions such as obesity and diabetes may also have contributed to an increased mortality burden in working-age US adults compared with their European counterparts34. Regarding global comparisons, the evidence for co-morbidity prevalence as an important predictor of cross-country COVID-19 mortality differences is still weak35.





One of the big takeaways for me about COVID is that, as a society, we didn’t learn a damn thing.
I have no confidence that if a guy like Trump was POTUS next time a deadly disease comes along we would do anything differently.
I would like to see a concerted Ad Council-style campaign to memorialize the fact that some large percentage of the 1.1 million dead Americans didn’t need to die – and only died because of “conservative” rhetoric, which was predicated on a cynical view that cities and “blue” areas would be hit harder than rural areas.
Somebody gets to write the history of COVID, and it’s high time the smart people step up to the task.
It is staggering to me that this isn’t a bigger deal – not just because of this study but because of the underlying fact that Trump killed hundreds of thousands of Americans thru his incompetence. Yet he and his Republican accomplices are given a pass.
@Tony W:
Of course they would.
They’d issue executive orders, or ram legislation through Congress if possible, banning lockdowns, capacity restrictions, and wearing masks in public. Later they’ll forbid any attempt to screen people with negative test results or vaccination.
Their base, and to be honest a lot more people as well, find restrictions and reduced economic activity, more onerous and offensive than piles of corpses.
Besides, who does Bulgaria think it is taking the number one spot in lowered life expectancy?
@daryl and his brother darryl:
This.
See my point on restrictions and economics vs piles of corpses.
But there’s more. It’s well known the 1918-20 flu pandemic killed tens of millions of people, and at a time of a much lower global population. yet we learn little about it in school, and there ins’t that much about it in more formal histories. One can say it has to compete for attention with WWI, but 1) it killed more people than the war, and 2) it was a factor in the war.
But there were also flu epidemics in the 1950s and 1960s that killed large numbers of people, and we hear literally nothing about it. they were nowhere near as bad as COVID, but they were pretty bad. We hear more about the polio outbreaks in the 50s, maybe because they led to reduced economic activity.
More interesting question to me is what happened in the places where the life expectancy drop reversed. I suspect that we don’t know the answer to that yet but haven’t read the article yet, either.
While I’m sure the Federal policies could have been much better, I really think that there are much greater factors at play.
– The most important is that nearly half of the people of this country have embraced anger, nihilism and anti-science as their prime motivators and lash out against anyone who tells them something they don’t want to hear. The negative effects are amplified because there are numerous enterprises (not just Fox) that market to these people by ginning up rage. It is further amplified by a major political party that has decided their hold on power is by riding on the coattails of all this.
– Any national health policy can only do so much because there are also 50+ state agencies and they have the prime responsibility to implement. They are also generating their own policies. It is inevitable that in this grab bag there are some that are seriously deficient, especially in the trump states where the populace has been trained never to expect anything from government.
– Finally, we don’t have national health care. In the better performing European companies the vaccine distribution and health messaging were provided by the same local doctors that people see for everything. Now that I think about it, this may be the biggest factor of all. There is a world of difference in having to make a special trip or a special appointment, and simply walking into the doctors office to complain about this or that random ache and having them say, “Alright then, it’s time for your booster.”
I’ve long contended that at the Federal level the US did about as good as we could expect. The things that made us perform so poorly compared to other nations were the things that were fundamentally different, and couldn’t be changed overnight.
I suspect good governance. You know, learning what works, what doesn’t, implementing the things that do and stopping the things that don’t?
@MarkedMan:
The executive branch, under Trump, did everything they could to sabotage the efforts against the virus and cause it to spread as quickly as possible. Trump literally held super-spreader events, including the one that killed Herman Cain, and the one that gave Trump COVID – some role model.
South Korea, by contrast, had their first case the same day as we did.
The U.S. has 4% of the world population and 16% of COVID deaths.
Leadership matters
@Kathy:
“They’d issue executive orders, or ram legislation through Congress if possible, banning lockdowns, capacity restrictions, and wearing masks in public. Later they’ll forbid any attempt to screen people with negative test results or vaccination.
Their base, and to be honest a lot more people as well, find restrictions and reduced economic activity, more onerous and offensive than piles of corpses.”
And the vast majority of such people loudly proclaim themselves to be pro-life, and expect us to take them seriously when they try to control women’s reproductive choices on that basis.
I’ll need to read the article, but it’s probable that a number of factors had an impact here. Example: fewer people on the roads meant fewer accidents, masking prevented additional diseases, staying at home prevented additional diseases, being more diligent about handwashing prevented additional diseases, factory closures meant fewer workplace injuries and/or deaths, and so on. With such a massive change in behaviors, there are likely dozens of factors that could have small impacts, with the end result being a change in life expectancy getting reversed.
@MarkedMan: Another potential contributing factor–connected with the lack of national health policy is the number of people who live in places where access to health care is low. I remember both my grandparents coming to Seattle periodically to see doctors of all sorts. Especially after the county hospital was converted to a nursing home when the last doctor who worked there retired. For lots of people, things haven’t changed on that front since the 60s.
@OzarkHillbilly: Considering that one of those points is “England/Wales,” color me skeptical on that good governance thing. 😉
@MarkedMan:
A problem in the US is that the healthcare system actively obstructs you from having a relationship with a physician. Yes, you may have the name of a PCP on your chart, but try and see that person, more often than not you’ll be shuffled off to a rotation physician assistants. For many folks, they likely have a more complete relationship with a pharmacist than they due they’re PCP.
@Tony W:
You are assuming the rest of the world has great reporting on covid deaths. Spoiler: many places do not.
@Sleeping Dog:
I had the same PCP from birth through college. When he retired, I moved on to a new PCP. The only reason I’m seeing a new one next week is that my current one is in the process of retiring.
Everyone I know sees their PCP, and has a long-term interaction with them. Hell… the one that’s retiring isn’t even “Dr. X” to me, he’s “Dave”.
@Mu Yixiao:
@Sleeping Dog:
Physician availability and insurance requirements (for the physician) can vary (capitation rates/capitation fees). My experience is more like Sleeping Dog’s (we are in the same state), with the only difference that I specifically book time with the PA/LPN rather than my PCP. I’ve literally never met the PCP to whom I am assigned (it’s changed a few times in recent years), but I’ve been seeing the same LPN for all of my appointments for around 7 years.
@Gustopher:
Oh, absolutely. Mexico, for instance, uses tests more to diagnose COVID than to prevent transmission. So I take those numbers with a big, giant, sack of salt. They’re at least double, and more likely far higher than that.
Then, too, I wonder how many deaths in the US, and elsewhere, due to COVID were reported as due to comorbidities. Physicians can be as political and partisan as anyone else.
But if overall deaths and case numbers are misreported on roughly similar rates all over, a very big IF, then the relative numbers still work out.
@Mu Yixiao:
For most of my adult life, my experience was similar to yours, but that changed significantly several years ago. When we moved to NH I got a new Doc and for about 10-12 years, I’d see him annually for a physical and as needed for, whatever. The one gripe I had, was that I couldn’t make an physical appt a year out, as they only booked out for 6 months. I’d set calendar reminder and call and set an appt, till one year, I called and was informed that my Doc didn’t have any physical slots available in the next 6 months, but I could see a PA. Since I didn’t care for the general practice and only went there for the Doc I saw, I went elsewhere. There in ~6 years I’ve had 3 different PCP’s and have to argue with them about seeing a MD rather than a PA for the physical, but I do see an MD.
My experience with my cardiologist is 100% different, they call me to set my annual and while I may spend time with a nurse at the appt. I always see the Doc. The weird thing is, both the cardio and the PCP are in the same general practice.
@Just nutha ignint cracker: HA! Touch’e.
@Sleeping Dog: I’ve been going to a clinic nearby for 20+ years now. Haven’t seen a doctor there in a long long time. I was seeing one particular Nurse Practitioner for most of that time (she saved my life at least once). Unfortunately she had a massive stroke, a real freak event, about 2 years ago. Since then it’s been catch as catch can as to who I see. They are all nice and very attentive but it would be nice if they could settle on one person.
As far as seeing a doc, I don’t miss that at all. The NPs all treat me like a person while doctors always like I was a data entry.
@Sleeping Dog:
To be fair, both my retiring PCP and the one I’ll be seeing are both PAs. For 99.44% of what I’m going for, that’s all I need. If something needs an MD to look at it, I get referred to one.
@Jen: I’m confused then. In my circumstance, a lot of the time the PA (sometimes BC) or the LNP that I see is listed on my insurance card as my PCP. Right at this moment, that is not the case because the practitioner that I see most often was hired too late in the previous year to have been listed as a PCP choice.
@Kathy: I often refer to this CDC site to look at excess deaths in the U.S. regardless of cause.
Many, many more people than usual died of all causes during COVID’s peak(s). Whether it’s directly from COVID or indirectly from full hospitals not having capacity to treat other conditions, really doesn’t matter.