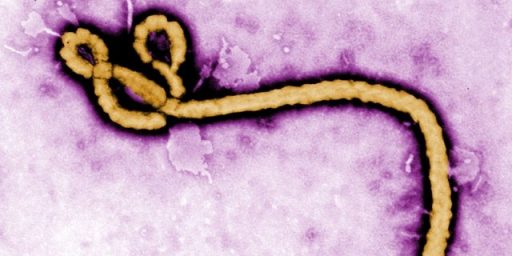
Battle Against Latest Ebola Epidemic Not Going Well
The response to the latest outbreak of the Ebola Virus has both succeeded and failed in several response.
The battle against the Ebola epidemic that has been gripping the Democratic Republic of Congo is not going well:
The family of a young woman who died from Ebola last month in the Democratic Republic of Congo dressed her body, put makeup on her face and propped her up in a car, hoping to make her look alive so they could drive her through checkpoints set up to prevent spread of the disease.
It was dangerous: Corpses are highly infectious. But they wanted to bury her in another town, next to her husband, who also had died of Ebola. Their desperate ploy failed. They were stopped at a checkpoint, according to a report from the country’s Ministry of Health.
The family’s flight, and apparent lack of understanding that bodily fluids spread the disease, help explain why this Ebola outbreak, in its seventh month, has become the second largest ever.
No end is in sight, despite the use of promising antiviral drugs and a vaccine that were not widely available in past epidemics. The deadliest outbreak occurred from 2014 to 2016, in Guinea, Liberia and Sierra Leone, and sickened 28,610 people and killed 11,308.
Last August, an unrelated outbreak began in the war-torn northeastern part of the Democratic Republic of Congo. So far, 907 cases and 569 deaths have been attributed to the disease, near the country’s borders with Rwanda, South Sudan and Uganda. The region has decent roads and a highly mobile population, experts said, so there is constant concern that the disease will spread to those countries.
More than 80,000 people have been vaccinated, and although hard data is lacking, experts suspect that without the vaccine, the epidemic would have grown much larger.
But efforts to stamp out the disease are failing in some areas because many people still don’t understand Ebola, and also because heavy-handed measures by outside organizations, local police and the military have alienated the communities, officials from aid groups and doctors who have worked in the region said. Fearful of being confined in isolation units, people have avoided testing and treatment. They do not want outside interference in rituals around death and burial.
“Ebola responders are increasingly being seen as the enemy,” Dr. Joanne Liu, president of Doctors Without Borders, said at a news conference in Geneva on Thursday. “In the last month alone, there were more than 30 different incidents and attacks against elements of the response.”
“The existing atmosphere can only be described as toxic,” she said.
Some people in the region question why the vaccine is being given only to certain people — including health workers and contacts of patients — and not to everyone, she said. Many wonder why outside aid has flooded in for Ebola, but not for malaria, diarrhea or other common, debilitating diseases that afflict many more people. Some have asked aid workers where they were when militias were carrying out massacres of civilians.
The northeastern part of the country where the epidemic has struck has been a conflict zone for decades, with more than 100 armed groups, as well as security forces posing a constant threat of violence to the population.
Distrust of outsiders is entrenched, and grew in two areas, Beni and Butembo, after the government barred residents there from voting in the long-delayed elections in December, supposedly because of concerns about the spread of Ebola. Many people thought the government had used the disease as an excuse to keep them from voting, and some of their anger turned against the outside groups that had drawn so much attention to Ebola.
Recent attacks on two treatment centers operated by Doctors Without Borders led the group to close them, and brought a scorching and highly unusual self-assessment by Dr. Liu, who included her organization among those that had fallen short. She urged medical teams to treat Ebola patients “as humans and not as a biothreat.”
(…)
In a piercing essay published on Thursday in The New England Journal of Medicine, another physician from Doctors Without Borders, Dr. Vinh-Kim Nguyen, wrote: “Early in the epidemic, we witnessed armed agents forcibly bringing patients in for treatment. In a population already traumatized by violence and forceful responses to numerous crises, such tactics fuel distrust of responders, which prompts patients to flee and spawns violence.”
Dr. Nguyen also noted that when Ebola teams were accompanied by security forces, they were met with fear and distrust, especially of forced vaccination. But when the security forces were absent, people would actually ask to be vaccinated.
“The lesson is clear: Guns and public health don’t mix,” he wrote.
Dr. Liu said aid groups needed to offer help in ways the community would accept, even if it meant helping families to safely care for Ebola patients at home, or giving them information and equipment to carry out safe burials on their own.
The key to stopping past epidemics had been to isolate the sick and track everyone who might have been exposed, until there were no more new cases. But that approach is not succeeding in Congo.
“More than 40 percent of the deaths are right now happening in the community,” outside of treatment centers, Dr. Liu said. “That means we have not reached them and they have not sought our care.”
It also means that untold numbers of people around these patients have been exposed and may have contracted the disease.
A spokesman for the World Health Organization, Tarik Jasarevic, confirmed that 40 percent of deaths were occurring in the community.
“But, and this is key, despite these worrying figures, the response has managed to bring the outbreak under control in 10 of 19 affected health zones, where there have not been cases in three weeks or more,” he said in an email. “The incidence numbers have dropped steadily since November. Clearly the response has had traction in these places, despite the challenges of community mistrust engendered by the years of conflict they have endured.”
But he also acknowledged that building trust was an important part of the work to be done.
“In every newly affected town, W.H.O. and partner social scientists and anthropologists work with local leaders to understand the context and tailor the approach to what works,” he said. As an example, he cited Beni, where the community had been hostile, but health workers were able to bring the outbreak under control within weeks.
In testing, the vaccine that has been developed against Ebola, which came about in no small part due to the concerted international effort to address the outbreak that occurred in western Africa in 2014, has been shown to be 100% effective in halting the spread of the disease. While this result is admittedly the result of controlled experiments under the supervision of public health professionals, even a success rate below 100%, but still respectably high, would be better than nothing, especially considering the nature of the disease and the ease with which it can spread in undeveloped countries such as the DRC where things like sanitation are faulty and long-standing customs regarding the handling of dead bodies actually ends up contributing to the spread of the disease.
Based on this report, it seems clear that the main problem that public health authorities are three-fold. First of all, it’s not nearly quite as easy to get beyond long-standing cultural practices and taboos that tend to make it easier for a disease like Ebola to spread as experts may have thought it was. Second, there appears to be a perhaps understandable skepticism about vaccination from people who aren’t sufficiently educated about the actual benefits (and risks) of vaccination in general and the Ebola vaccine in particular. Finally, it appears from the reports that the DRC authorities have been utilizing heavy-handed tactics in an effort to force public compliance. This last development seems like a mistake. A better option would be to educate the populace more effectively. These people can already see the impact that Ebola is having on their communities, but forcing them to comply with public health orders at the point of a gun is probably not the best way to get people to cooperate, and more likely to make people suspicious of public health authorities, physicians, nurses, and others attempting to deal with this serious health problem.
The good news, if there is any good news, is that the latest outbreak appears to be staying within a relatively limited geographic area. The first reports of an outbreak in the DRC came out in the spring of 2017. Last spring, it became apparent that the 2017 outbreak had not been suppressed as easily as previously thought and there were signs that it had hit a major city in the DRC. While those are serious issues, it does not appear that the disease has spread beyond that area, or outside the DRC in the time since then. This is in stark contrast to the 2014 western Africa outbreak, which spread quickly to three nations and also managed to make it, in limited cases, as far as the United States and Europe, although nearly all of those cases were caught early enough that the patients were cured of the disease. To that extent, one could arguably say that the public health response to this outbreak has been a huge success, but that’s hardly sufficient for the people of the DRC who are still under threat. They need better policies and approaches than what we’re seeing now if Ebola is going to be defeated there.